This guide will teach you the signs of a Traumatic Brain Injury (TBI) that most doctors miss and how to treat your brain injury.
Have you ever felt “off” after a fall, accident or a hit to the head—like your brain isn’t working the way it used to?
You’re not alone. Millions of people suffer from traumatic brain injuries (TBIs) each year—many without ever realizing it.
A TBI injury can affect your memory, mood, sleep, balance and even change your personality. But here’s the good news: there is hope—and healing is possible.
At Genesis Brain Institute in Tampa, our brain treatment center specializes in helping people identify, understand and recover from traumatic brain injuries using advanced diagnostics and personalized, drug-free brain treatment programs.
First: Take the TBI Symptoms Quiz: A Free, Easy First Step
If you feel you could be dealing with a brain injury and not even know it, this is your moment of clarity.
We created a quick, free quiz to help you screen for symptoms of a traumatic brain injury.
It takes less than two minutes and can help determine whether you should come in for a full evaluation at a trusted brain treatment center.
Many people ignore symptoms like brain fog, irritability or dizziness, thinking it’s just stress or aging — when in reality, their brain is still trying to recover from a past trauma.
If you don’t live in the Tampa area and have experienced a fall, car accident, sports injury or emotional trauma, this quiz is a smart place to start.
Now let’s get into everything you should know about Traumatic Brain Injuries.
What Is a Traumatic Brain Injury?
A traumatic brain injury happens when an outside force disrupts the normal function of your brain.
This can be caused by:
- A direct blow to the head (from sports, accidents or a fall)
- A sudden change in motion (such as a whiplash-type injury)
- Blast waves or combat exposure (common in veterans and law enforcement)
- Repetitive low-level head impacts (seen in athletes)
The result is often called an alteration of consciousness—meaning you may feel confused, disoriented or even black out.
But even without losing consciousness, a traumatic brain injury can still occur.
TBIs are generally classified by severity:
- Mild (Concussion) – No or brief loss of consciousness; often no visible findings on scans
- Moderate – Longer confusion, loss of consciousness for up to 5 minutes or visible changes on imaging
- Severe – Extended unconsciousness, major neurological symptoms and lasting impairment
It’s important to know that you do not need to lose consciousness to have a concussion. That’s an outdated myth. In fact, the majority of concussions happen without any blackout at all.
TBI Symptoms: What to Watch Out For
One of the most overlooked aspects of a traumatic brain injury is how delayed and subtle the symptoms can be.
Many people walk around for months—or even years—without realizing their headache, anxiety or poor memory could be tied to a past fall, car accident, sports injury or even emotional trauma. These symptoms often get brushed off as aging, burnout or just a “rough patch.”
But what if it’s your brain asking for help?
Here’s what to look for.
Cognitive Symptoms (Thinking, Memory and Focus)
- Trouble concentrating or staying focused
- Short-term memory lapses (forgetting names, dates, appointments)
- Slower processing speed (taking longer to think or respond)
- Difficulty making decisions or planning tasks
- Trouble finding the right words (word-finding difficulty)
These signs can sneak up slowly. You might find yourself reading the same paragraph over and over, forgetting why you walked into a room or struggling to stay engaged in a conversation.
Emotional and Behavioral Symptoms
- Increased irritability or sudden mood swings
- Anxiety or panic that wasn’t there before the injury
- Depression or lack of motivation
- Emotional numbness or flat affect
- Difficulty managing stress
One of the most common things we hear at Genesis Brain Institute is:
“I just don’t feel like myself anymore.”
This is especially true for people who used to be calm, upbeat, or driven—only to find themselves snapping at loved ones or withdrawing socially.
Physical Symptoms
- Persistent headaches or pressure in the head
- Dizziness, vertigo, or lightheadedness
- Nausea or sensitivity to motion
- Blurry or double vision
- Sensitivity to light or noise
- Balance problems or difficulty with coordination
- Ringing in the ears (tinnitus)
Some people also experience fatigue that doesn’t go away with rest—what we call post-concussive fatigue.
It’s your brain trying to function while working overtime to compensate for injury.
Sleep Disturbances
- Trouble falling asleep
- Waking up throughout the night
- Sleeping too much and still feeling tired
- Nightmares or vivid dreams
Poor sleep not only slows recovery, but can also worsen symptoms like anxiety, irritability and brain fog.
When Symptoms Don’t Go Away
In many cases, mild TBI symptoms improve on their own within a few days or weeks. But for roughly one-third of patients, symptoms linger—and sometimes intensify. This condition is called Post-Concussion Syndrome (PCS).
Post-Concussion Syndrome can last weeks, months or even years, especially if the brain hasn’t been properly diagnosed and treated. Some people go from doctor to doctor without answers, even being told “it’s all in your head.”
That’s why we created the TBI Symptoms Quiz—to give you a clear and credible first step in understanding what your brain may be experiencing.
TBI Symptoms Often Overlap With Other Conditions
A traumatic brain injury can mimic or worsen other mental health and neurological issues, including:
- ADHD or attention challenges
- Depression and anxiety disorders
- PTSD (Post-Traumatic Stress Disorder)
- Bipolar disorder
- Chronic fatigue syndrome
- Fibromyalgia
- Migraine disorders
- Early cognitive decline or brain fog
That’s why many people are misdiagnosed or underdiagnosed, especially if they never connected the dots between their current symptoms and a head trauma that happened months or years earlier.
It’s not uncommon for us to see someone who was diagnosed with ADHD or anxiety in their 30s or 40s—but who had a childhood sports injury or recent car accident that was never properly evaluated.
Diagnosing Traumatic Brain Injury: Why “Normal” Scans Miss So Much
One of the most frustrating experiences for people with a traumatic brain injury is being told, “Your scan looks fine.”
You walk into the ER or your primary care doctor’s office with TBI symptoms that are very real—and yet your MRI or CT scan comes back “normal.”
So what gives?
The truth is this:
Standard imaging looks at structure, not function.
And most mild TBIs—including concussions—don’t show up on structural scans.
If your brain isn’t bleeding or visibly damaged, it will often be declared “normal,” even if your day-to-day life feels anything but.
At Genesis Brain Institute in Tampa, our brain treatment center takes a different approach. We use advanced diagnostics that look beyond structure—into the functionality, communication and coordination of your brain.
Here’s how we uncover what’s really going on.
1. Detailed Clinical History: Understanding the “Before and After”
Before we touch any machines or run any tests, we start by listening.
We want to understand:
- What happened leading up to the injury
- How your brain and body felt immediately after
- What symptoms have lingered or worsened
- What has changed in your work, family life, memory or personality
We also ask questions to assess any past trauma, childhood injuries or emotional stressors that could compound the brain’s current state.
This clinical context allows us to piece together the full picture—not just snapshots in isolation.
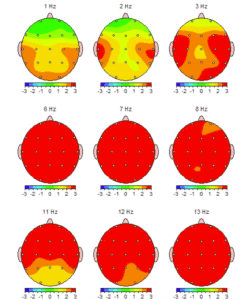
2. qEEG Brain Mapping: Seeing the Brain’s Electrical Signature
Your brain is powered by electricity.
It communicates through electrical waves that travel across different regions and networks. When you experience a brain injury, those electrical signals can become irregular, disrupted or out of sync.
Quantitative Electroencephalography (qEEG) lets us measure that electrical activity and map it—just like a GPS for your brain.
Why it matters:
- It shows us which brain regions are underperforming, overcompensating or dysregulated
- We can identify patterns like too much slow-wave activity (brain fog, fatigue) or excessive fast waves (anxiety, insomnia)
- It compares your brain against a large database of age-and gender-matched “normative” brain activity
The result of a qEEG brain map, is a color-coded brain map that reveals what traditional imaging misses. Instead of guessing, we get data-backed direction.
We often find that patients with clean MRIs still have frontal lobe dysregulation, overactivity in the visual cortex or imbalanced networks that explain their memory loss, irritability or sleep issues.
3. Video Oculography (VOG): Your Eyes Reveal Your Brain’s Secrets
Your eyes aren’t just windows to the soul—they’re directly connected to your brainstem and cerebellum.
Using Video Oculography, we track your eye movements with high-speed infrared cameras to evaluate:
- How your eyes move from one point to another (saccades)
- How smoothly they follow a moving object (smooth pursuit)
- How your pupils respond to light
- How well your eyes coordinate with your vestibular (balance) system
These movements reflect activity in specific brain regions.
For example:
- Poor smooth pursuit can point to frontal lobe dysfunction
- Pupil delays may indicate autonomic nervous system dysregulation
- Saccade errors can reveal cerebellar imbalance
This type of insight is critical when treating issues like balance problems, dizziness, headaches or blurry vision—all common after TBI.
4. Autonomic Nervous System Testing: Is Your “Fight or Flight” Stuck On?
Your autonomic nervous system (ANS) controls everything you don’t think about—like heart rate, blood pressure, breathing, digestion and pupil size. After a traumatic brain injury, many people’s ANS becomes dysregulated—stuck in “fight or flight” mode.
We assess signs of this using:
- Pupillometry (pupil size and response to light)
- Heart Rate Variability (HRV)
This testing helps us determine whether your anxiety, insomnia or digestive problems are coming from emotional trauma, brainstem dysfunction or both.
5. 12-Domain Cognitive Testing: Targeting the Right Deficits
A one-size-fits-all “memory test” doesn’t cut it when it comes to brain injury.
At Genesis, we break cognition into 12 specific areas so we can pinpoint exactly what’s being affected.
These include:
- Episodic Memory: Can you recall events, faces or facts from the past?
- Working Memory: Can you hold information in your mind while using it?
- Visual-Spatial Memory: Can you navigate physical space or recall what you see?
- Verbal Memory: Are you struggling with names, vocabulary or reading retention?
- Processing Speed: Is everything taking longer—reading, reacting, thinking?
This breakdown lets us craft a brain treatment plan—so we’re not just training your brain blindly, but strengthening the exact circuits that need it.
Why This Matters in Tampa and Beyond
We often work with clients from Tampa, St. Petersburg, Clearwater, Brandon, Wesley Chapel, Orlando and across Florida who have spent years searching for answers.
They’ve seen neurologists nearby, psychiatrists and general practitioners—but no one connected the dots.
Once they go through our full brain diagnostic process, they finally feel seen—and finally understand why they’ve felt “off” for so long.
You can’t treat what you don’t measure. And you can’t measure what you’re not looking for.
A Personalized Path to Recovery: How We Treat Traumatic Brain Injuries at Genesis Brain Institute (Tampa, FL)
No two brains are the same.
No two brain injuries are the same.
So why do so many brain treatment plans still look the same?
At Genesis Brain Institute, we believe in precision-guided, personalized care.
Once we’ve completed a full diagnostic workup—including qEEG brain mapping, eye tracking, cognitive testing and autonomic analysis—we build a brain treatment protocol that reflects your needs, your goals and your brain function.
Here are the brain treatment modalities we use most often to help people in Tampa recover from concussions, TBIs and post-concussive syndrome—without relying on long-term medication.
Hyperbaric Oxygen Therapy (HBOT)
What it is:
A non-invasive treatment where you sit or lie in a special chamber and breathe 100% pure oxygen at increased atmospheric pressure.
Why it helps:
After a brain injury, blood flow is often disrupted—and the oxygen that cells need for healing can’t get where it needs to go. HBOT therapy increases the amount of oxygen your blood can carry and helps it reach damaged or dormant tissue.
Benefits include:
- Faster recovery of cognitive function
- Improved memory and attention
- Reduced inflammation in brain tissue
- Stimulation of new blood vessel and neuron growth
What to expect:
Many patients report increased mental cognition, better sleep and fewer headaches within a few sessions.
It’s painless, quiet and often deeply relaxing.

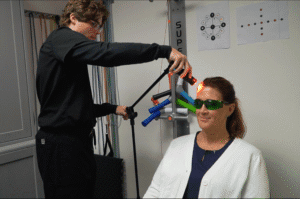
Photobiomodulation (PBM)
What it is:
A safe, evidence-based therapy that uses red and near-infrared light to stimulate cellular healing in the brain.
Why it helps:
After a TBI, the brain can lose energy at the cellular level. PBM targets mitochondria (your cells’ energy engines) and helps restore normal metabolism and blood flow.
Benefits include:
- Boosted mental energy
- Sharpened memory and focus
- Reduced brain inflammation
- Improved mood
What to expect:
A light-emitting cap or headset is placed on your head for several minutes. Most patients feel relaxed during the session, with cumulative improvements over time.
Neurofeedback
What it is:
Neurofeedback watches your brain activity in real-time and trains it toward healthier patterns—just like physical therapy for your mind.
Why it helps:
Brain injuries can create abnormal wave patterns—like too much slow activity (brain fog) or too much fast activity (anxiety). Neurofeedback helps your brain correct those patterns.
Benefits include:
- Better attention and focus
- Improved emotional regulation
- Fewer mood swings
- Reduced reliance on medications
What to expect:
Sensors are placed on your scalp and you’ll watch a movie, show or game that responds to your brain waves. When your brain moves toward a healthy state, the screen stays bright and clear. When it drifts off, the screen dims or pauses.
Your brain learns to optimize itself—no pain, no electricity, no side effects.
Transcranial Magnetic Stimulation (TMS Treatment)
What it is:
A non-invasive procedure that uses targeted magnetic pulses to stimulate specific brain regions involved in mood, focus and memory.
Why it helps:
TMS therapy is FDA-approved for depression and now widely used for post-concussive symptoms, including brain fog, fatigue and emotional instability.
Benefits include:
- Activation of underperforming brain regions
- Reduction in depression and anxiety symptoms
- Long-lasting neuroplastic changes
- No systemic side effects
What to expect:
You sit in a comfortable chair while a small magnetic coil delivers precise pulses to your scalp. Sessions are typically 20–30 minutes and can be completed over a few weeks.
Vestibular and Eye Movement Rehabilitation
What it is:
Targeted therapy for dizziness, balance issues and visual instability—common after head trauma.
Why it helps:
The vestibular system (inner ear and brain connections) often gets disrupted during TBI injuries. Eye tracking problems can lead to headaches, dizziness and difficulty reading or focusing.
We use:
- Head-turn exercises
- Balance board training
- Gaze stabilization drills
- Eye convergence and tracking routines
What to expect:
This brain therapy is tailored to your specific deficits based on your VOG results. Many people find balance, stability and visual comfort improves within weeks.
Cognitive Rehabilitation and Brain Training
What it is:
Computerized and therapist-guided exercises designed to rebuild memory, attention, processing speed and executive function.
Why it helps:
Cognitive rehab targets the exact domains identified in your evaluation—whether it’s spatial memory, working memory or information recall.
Benefits include:
- Sharper thinking
- Faster reaction times
- Stronger multitasking ability
- Greater confidence at work, school or home
What to expect:
We use gamified platforms and real-world training exercises to make it engaging. Your results are tracked over time to see measurable progress.
Virtual Reality Biofeedback
What it is:
An immersive therapy combining VR and physiological feedback tools (like heart rate variability monitors) to train emotional control and nervous system regulation.
Why it helps:
A TBI injury often disrupts the autonomic nervous system—leading to anxiety, panic or feeling “on edge.” VR biofeedback helps recalibrate your stress response.
Benefits include:
- Reduced anxiety and panic
- Better heart rate control
- Calmer responses to stressors
- Improved emotional flexibility
What to expect:
You’ll wear a VR headset while interacting with guided environments, games or relaxation scenes that respond to your breathing and heart rhythms.
This teaches your body how to stay regulated even under pressure.
Emotional and Mental Health Support
Trauma doesn’t just affect the brain physically—it affects you emotionally, spiritually and relationally.
We work alongside:
- Licensed mental health counselors
- Psychologists and psychiatrists
- Faith-based therapists
We also incorporate powerful tools like:
- EMDR Therapy (Eye Movement Desensitization and Reprocessing)
- Cognitive Behavioral Therapy (CBT)
- Neurofeedback and TMS for emotional regulation
These therapies are especially important for patients with co-occurring PTSD, grief or emotional trauma related to their injury.
TBI and PTSD: The Overlooked Connection That Could Be Slowing Your Recovery
It’s not just in your head—well, actually, it is.
But the reason you can’t sleep, feel constantly on edge or startle at loud sounds might not be just psychological. For many patients, it’s the result of both a traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) happening at the same time.
And when these two conditions overlap, recovery gets more complicated—but not impossible.
At Genesis Brain Institute, we work with a wide range of individuals in Tampa and beyond who have experienced both TBI and PTSD—from car accident survivors and first responders, to veterans, athletes and survivors of abuse. Often, their trauma is layered—physical, emotional and neurological all at once.
Here’s what you need to know.
How TBI and PTSD Are Connected
A traumatic brain injury disrupts how your brain processes signals.
PTSD disrupts how your brain processes memories, emotions and danger.
When you combine the two, your nervous system can stay stuck in “high alert” mode while your brain struggles to regulate itself.
This creates a vicious cycle:
- You can’t sleep because your mind won’t calm down
- You can’t think clearly because your fear centers are overactive
- You can’t heal emotionally because your brain isn’t able to process trauma normally
Even if you don’t remember the traumatic event clearly (because of a concussion or blackout), your limbic system—the part of your brain responsible for emotions and memory—might still be reacting as if it just happened.
Common Signs You May Have Both TBI and PTSD
- Nightmares or vivid, disturbing dreams
- Flashbacks or intrusive memories
- Heightened startle response (jumping at noises, feeling tense)
- Panic attacks or shortness of breath
- Avoiding people, places, or situations that trigger memories
- Emotional numbness or frequent outbursts
- Trouble sleeping or staying asleep
- Feeling “on edge” all the time
- Dissociation or memory gaps around the traumatic event
It’s important to understand that not all people with TBI have PTSD, and not all people with PTSD have had a brain injury—but when the two conditions co-exist, healing requires a highly specialized approach.
How We Treat TBI and PTSD Together at Genesis Brain Institute
This is where our integrative model shines.
Because we’re not only mapping the neurological dysfunction, but also caring for the emotional and psychological impact, we’re able to craft a brain treatment plan that targets both layers of a brain injury.
Step 1: Identify the Source
Again, as mentioned above, we use tools like a qEEG brain map and autonomic nervous system testing to see whether your symptoms are coming from:
- Limbic system overactivation (emotion and fear centers)
- Frontal lobe underfunction (decision-making, calm reasoning)
- Brainstem dysregulation (fight-or-flight control center)
- Visual and sensory system overload
Step 2: Stabilize the Brain
We begin with interventions that help calm the nervous system and restore balance:
- Neurofeedback: Calms overactive fear circuits and helps rewire regulation patterns
- TMS (Transcranial Magnetic Stimulation): Targets areas like the dorsolateral prefrontal cortex, known to help with depression and emotional regulation
- HRV (Heart Rate Variability) Training: Retrains the autonomic system to shift from fight-or-flight into rest-and-digest mode
Step 3: Process the Trauma
We work with our licensed trauma-informed therapists trained internally in:
- EMDR Therapy: A gold-standard treatment for PTSD that helps reprocess traumatic memories using guided eye movements
- Cognitive Behavioral Therapy (CBT): To reframe and manage negative thought patterns
- Faith-based counseling: For patients who want to integrate spiritual healing into their journey
Step 4: Rebuild from the Inside Out
Once the brain is stabilized and trauma is being addressed, we layer in:
- Cognitive rehabilitation
- Photobiomodulation for emotional resilience
- HBOT for neuroinflammation tied to stress
- Virtual reality exposure therapy for real-time emotional training
Traumatic Brain Injury Survivor Story
Why This Matters Tampa
First responders, veterans and active-duty military personnel in the Tampa Bay area are at particularly high risk for combined TBI and PTSD.
Also at high risk for combined TBI and PTSD Injuries:
- Domestic abuse survivors
- Car crash victims
- Athletes with repeated head injuries
- Children or teens with complex trauma (foster children)
We’re here to tell you:
You are not broken.
Your brain just needs support.
Healing is possible when you treat both sides of the brain injury—the emotional and the neurological.
Living in Tampa with a Brain Injury? Here’s What to Do Next
If you’re reading this and thinking, “This sounds like me,”—trust that instinct.
Whether you’ve been quietly struggling for months or you’ve bounced between doctors without answers, your brain may be telling you that something deeper is going on.
You’re not weak.
You’re not alone.
If you live in Tampa, St. Pete, Wesley Chapel, Brandon, Clearwater, New Port Richey or anywhere in the Tampa Bay area, we’re here to help.
What if I Don’t Live in Tampa?
We work with patients from all over the country—and even internationally—who are searching for answers after head injuries, concussions, car accidents or long-term cognitive decline symptoms.
Many out-of-town clients stay right here in our business park, just steps from our brain treatment center and minutes from the Tampa International Airport (TPA).
You’ll have convenient access to two nearby hotels outside our office doors on the water:
- The Westin Tampa Bay – A restful, luxury hotel located right on the water, offering spacious rooms and a peaceful atmosphere ideal for healing and recovery
- The DoubleTree by Hilton Rocky Point – A trusted, comfortable option with extended-stay amenities and beautiful views of Tampa Bay—perfect for families or longer programs
Whether you’re flying in for a one-time brain diagnostic evaluation or committing to a multi-week healing protocol, we make it easy to get the care you need—even if you don’t live in Florida.
Our team will gladly help you coordinate logistics, provide hotel information best for you and your care schedule so you can focus on what matters most: healing your brain and restoring your life.
We don’t do guesswork. We don’t hand you a bottle and say, “Let’s see if this works.”
We test. We map. We track. And we treat your brain with the same care we’d want for our own families.
Here’s how to take the first step:
1. Start with the Free TBI Symptoms Quiz
If you’re not sure whether you’ve had a brain injury—or if your symptoms “count”—this quiz is your starting point. It’s short, powerful and confidential.
2. Book a Brain Consultation
If your quiz results suggest possible TBI-related dysfunction (or you feel off), schedule a consultation with our clinical team. We’ll review your history, answer your questions and recommend next steps.
3. Get Your Brain Map
From there, we’ll create your custom diagnostic plan, which may include:
- qEEG Brain Mapping
- Cognitive Testing
- Eye Movement Analysis
- Nervous System Evaluation
4. Begin a Brain Treatment Plan That’s Built for You
You’ll receive a personalized brain treatment plan backed by your unique data—not a generic checklist.
Final Takeaways: There Is Real Hope for Healing
A traumatic brain injury can leave you feeling like a shadow of yourself. The sharpness fades. Your mood shifts. Relationships strain. People say “you look fine,” but you know—deep down—you’re not.
That’s not a weakness.
That’s your brain asking for help.
And we want you to know this:
- You don’t need to suffer in silence.
- You don’t need to settle for “normal” scans that miss the deeper story.
- You don’t need to stay stuck in the fog.
There is a path forward. There are therapies that work. There are people who will listen, believe you and walk with you—step by step—until the light comes back on.
Your brain can change. Your symptoms can improve. Your life can be restored.
If you’re in the Tampa Bay area and ready to finally get answers and a plan that actually fits you, we’re here.
Because at Genesis Brain Institute, we don’t just treat brains—we serve people.
And your healing story is just getting started.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Please consult with a licensed healthcare provider. Genesis Brain Institute is a Brain Treatment Center in Tampa offering non-pharmaceutical solutions that bring clarity, restore function, and offer real hope for those who feel lost, stuck, or simply want more from life.