Rehabilitation for brain injuries begins with understanding what most scans miss. Every week at Genesis Brain Institute in Tampa, we meet people who are still suffering months after a car accident, yet every doctor has told them the same thing. “Your MRI looks normal. You should be fine.”
But they don’t feel fine.
They feel foggy, forgetful, anxious, and frustrated that no one can explain why their life changed after the crash. Many don’t realize that their symptoms aren’t “in their head.” They are inside their brain’s electrical networks, the part of brain function MRI and CT cannot measure.
At Genesis Brain Institute, our rehabilitation approach is built around the advanced work of Dr. Emily Kalambaheti, Director of Rehabilitation and a featured presenter at a major neurology conference, where she shared a clinical case study on traumatic brain injury (TBI) using qEEG Brain Mapping in Tampa.
Her research highlights a truth most accident survivors never hear:
One in three drivers will get a TBI from a car accident.
And the majority of these injuries do not appear on MRI or CT because concussions happen at the cellular and electrical level. When traditional scans show “nothing,” people are left suffering without answers.
qEEG Brain Mapping changes that.
It reveals the slowed brainwaves, network disruption, and suppressed processing speed that drive symptoms like brain fog, headaches, visual strain, balance issues, memory problems, and anxiety.
And when qEEG guides a personalized rehabilitation plan, recovery becomes possible. In Dr. Kalambaheti’s case study, a patient saw a 40% improvement in symptoms and measurable changes in brain function after a multi-modal rehabilitation program at Genesis Brain Institute.
If you are still struggling after a car accident, this matters for one reason:
Your brain can change. And with the right rehabilitation plan, you can too.
In this case study, we’ll cover:
✔ What happens inside the brain during a car accident
✔ Why MRI and CT scans miss so many brain injuries
✔ How qEEG Brain Mapping detects hidden dysfunction
✔ The exact abnormalities seen in the Tampa patient’s brain
✔ The multi-modal rehabilitation program used at Genesis Brain Institute
✔ How his symptoms improved by 40%
✔ Why this approach brings measurable hope to TBI survivors
By the end, you’ll understand why so many people feel “off” after a crash —and how a data-driven, personalized, and compassionate rehabilitation plan can help you feel like yourself again.
What Happens to the Brain After a Car Accident?
When someone is involved in a car accident, the brain can move suddenly inside the skull. Even without a direct hit to the head, this quick back-and-forth motion stretches delicate neural tissue. Dr. Kalambaheti explained that all concussions are traumatic brain injuries, but not all traumatic brain injuries look dramatic on the outside. Car accidents are one of the most common causes of hidden brain injuries. During her presentation, she shared a statistic most people never hear:
One in three drivers will get a TBI from a car accident. This means millions of people walk away from a crash appearing “fine,” but their brain has experienced a sudden, invisible change that affects how they think, feel, and function.
Why These Injuries Are So Hard to See
Dr. Kalambaheti emphasized that concussions and mild TBIs often do not show up on MRI or CT scans. These tools are excellent for detecting major problems like bleeding or fractures, but they cannot see stretched neural pathways, disrupted electrical activity, or changes in how brain networks communicate. A concussion is not simply a bruise. It is a disturbance in how the brain’s electrical systems work. Because the injury is functional instead of structural, MRI and CT frequently appear normal even when the person has headaches, fogginess, memory difficulties, dizziness, or anxiety. This is why so many patients are told “Nothing is wrong,” yet continue to suffer.
What Happens Inside the Brain’s Electrical System
To understand what changes after a car accident, Dr. Kalambaheti explained how healthy brainwaves work. The brain communicates through electrical signals that fall into different frequency bands: delta, theta, alpha, beta, and gamma. Each wave type plays a distinct role in thinking, attention, memory, and emotional regulation. After a traumatic brain injury, these waves can shift dramatically.
Based on what she sees with her TBI patients, car-accident-related injuries often show:
1. Elevated Slow Waves (Delta + Theta): This makes people feel foggy, tired, or slowed, like their brain can’t think fast enough. Patients often say, “I know what I want to say, but I can’t get the words out,” or “I remember meeting you, but I can’t recall your name.”
2. Reduced Fast Waves (Beta): This affects problem-solving, processing speed, and the brain’s ability to stay organized.
3. Alpha Shifts: Alpha waves, normally dominant in the back of the brain, may shift forward after a concussion, contributing to visual strain or mood-related symptoms.
4. Coherence Problems: Coherence is how well different brain regions communicate. After TBI, Dr. Kalambaheti often sees hypercoherence, especially in the first one to two years post-injury. Hypercoherence is when the brain is “over-connected,” creating too much crosstalk. It shows the brain is trying to reorganize and stabilize itself but struggling to do so efficiently.
Why Symptoms Linger
When the brain produces too much slow wave activity and not enough fast wave activity, combined with disrupted communication between regions, daily life becomes harder. Focusing takes more effort, conversations feel overwhelming, memory slips under stress, vision strains easily, balance feels inconsistent, and anxiety increases because the nervous system is dysregulated. These symptoms are not imagined. They come directly from measurable changes in the brain’s electrical activity.
And because every brain is unique, Dr. Kalambaheti explains that every injury is unique as well. Two people can have the same crash and walk away with completely different patterns of disruption. That is why each person needs a rehabilitation plan based on their brain’s specific changes, not a generic, one size fits all approach.
This leads to the next crucial question:
If a MRI can’t see these injuries, how do we find them?
That’s where qEEG Brain Mapping becomes essential.
Why MRI and CT Scans Miss So Many Brain Injuries
One of the most confusing moments for people after a car accident is hearing that their MRI or CT scan “looks normal,” even though nothing about their daily life feels normal. Dr. Kalambaheti explained that this happens because traditional imaging looks for structural problems, things like fractures, bleeding, swelling, or large lesions. These tools are excellent at catching major damage, but most concussions and mild traumatic brain injuries do not cause structural changes big enough to be seen on these scans.
A concussion is an injury that happens at the cellular level. When the head moves suddenly, the brain stretches, twists, or shears microscopic pathways inside the tissue. These pathways carry electrical signals that help the brain think, remember, feel, and process the world. Even small disruptions in these pathways can create big changes in how someone functions.
But because this type of injury is about electrical disruption, not structural destruction, MRI and CT scans often show “nothing wrong.” This leaves patients confused, discouraged, and sometimes even doubting their own symptoms.
Dr. Kalambaheti also noted practical limitations. CT scans expose patients to radiation. MRIs can be difficult for individuals with metal implants, certain pacemakers, or spinal cord stimulators. She also sees many veterans who avoid an MRI because the narrow tube, loud noise, and long stillness trigger claustrophobia or PTSD symptoms. When someone cannot tolerate or safely undergo an MRI, important information can be missed.
Even when MRI or CT scans are available and clear, they cannot measure:
electrical communication between brain regions
the speed of brain processing
abnormal brainwave patterns
network disconnects or overloads
how different parts of the brain synchronize
These are the exact changes that cause brain fog, dizziness, memory problems, anxiety, irritability, or slow thinking after a concussion.
Dr. Kalambaheti emphasizes that a lack of MRI findings does not mean a lack of TBI. Someone can have real symptoms, real functional impairment, and real neurological change, even when their scan looks perfectly normal.
This is why so many patients feel dismissed. They are told, “Everything looks fine,” but they continue struggling through daily life with symptoms that clearly are not fine. Their injury simply exists in a part of the brain that MRI and CT cannot see.
What they need is a way to measure the brain’s electrical activity, the part that governs how the brain actually functions. This is exactly where qEEG Brain Mapping comes in.
How qEEG Brain Mapping Detects Hidden Brain Dysfunction
qEEG Brain Mapping gives us something MRI and CT cannot: a direct look at how the brain is functioning. While MRI shows structure, qEEG shows communication, how brain regions talk to each other, how fast or slow they are working, and whether the electrical signals are balanced or disrupted.
During her presentation, Dr. Kalambaheti explained that a qEEG starts with a standard EEG recording. She uses a cap with 19 electrodes placed across the scalp to measure the brain’s electrical activity. An EEG produces lines and squiggles that neurologists have studied for decades, but the real power comes when those electrical signals are transformed into a visual map.
This is where the “quantitative” part comes in. The data from the EEG is fed into mathematical algorithms that convert raw electrical activity into topographical maps. These maps show the intensity of brainwaves in different regions and highlight where the brain is producing too much activity, too little activity, or struggling to stay in sync.
qEEG provides objective metrics that reflect the brain’s real-time behavior. Dr. Kalambaheti looks closely at several key areas:
Power: The strength of each brainwave type (delta, theta, alpha, beta). Abnormal power levels can point to fogginess, slowed thinking, mood changes, or processing difficulties.
Coherence: How well different brain regions communicate. Too much coherence or too little coherence reveals network dysfunction.
Phase: How quickly signals travel between regions and whether they arrive too early or too late.
Asymmetry: Differences between the left and right sides of the brain, which can influence emotion, attention, and processing.
She compares each patient’s results to a large normative database based on healthy individuals of similar age, gender, and handedness. This comparison highlights exactly where the brain has shifted away from normal patterns. Just like bloodwork uses reference ranges, qEEG uses reference norms to show what is typical and what is not.
qEEG is especially valuable in a traumatic brain injury because the electrical abnormalities that follow concussions happen long before structural changes would ever appear.
After a TBI, the brain may show elevated slow waves, reduced fast waves, and abnormal coherence patterns that reflect the injury’s impact on functional networks.
These patterns explain why someone may feel foggy, slow, overwhelmed, emotional, or mentally tired even though their MRI looks normal. The injury is real, it just exists in a part of the brain that requires a different tool to measure.
Dr. Kalambaheti uses these maps to not only confirm the presence of an injury but also to guide rehabilitation. By identifying which regions are underperforming and which networks are overworking, she can build a brain rehabilitation plan that is targeted, efficient, and personalized. Each treatment session is shaped around the individual’s unique brain map.
qEEG makes the invisible visible. It takes the mystery out of symptoms and gives patients something they desperately need after a traumatic brain injury: clarity.
Inside the Patient’s Brain: What the qEEG Revealed in This Tampa Case Study
When the patient arrived at Genesis Brain Institute two months after his car accident, he was still struggling with headaches, eye strain, visual disturbances, balance problems, forgetfulness, anxiety, and musculoskeletal pain. Even though he had lost consciousness during the crash, his imaging did not reveal any major structural damage. Yet his symptoms were affecting him every single day.
To understand what was happening inside his brain, Dr. Kalambaheti recorded a 19-channel EEG and converted it into a qEEG Brain Map. This brain map revealed several clear indicators of traumatic brain injury, patterns she frequently sees in individuals recovering from car accidents.
The first major finding was elevated slow-wave activity, particularly in delta at one hertz and theta at four hertz. These increases in slow waves are common in TBIs and often match how patients feel after a concussion. When the brain produces too much slow wave activity, people describe fogginess, mental fatigue, trouble recalling names, or difficulty pulling words out when speaking. This patient’s symptoms aligned exactly with what the qEEG showed.
The second key finding was a decrease in beta activity, especially high beta between 21 and 25 hertz. Beta waves support faster thinking, processing, and organization. When these waves are suppressed, people feel like they cannot think quickly or clearly. Everyday tasks take more effort, and problem solving becomes slow and tiring. This patient’s reduced beta activity matched his reports of cognitive difficulty and overwhelm.
A third finding involved alpha activity, which typically appears strongest in the back of the brain. After head injuries, alpha patterns can shift forward or appear abnormal, contributing to visual strain or difficulty calming the mind. This pattern is often seen in both concussions and mood conditions, and it played a role in this patient’s ongoing symptoms.
Finally, the qEEG revealed a significant pattern seen in many post-accident patients: hypercoherence. Coherence reflects how well different parts of the brain communicate. After a TBI, the brain may become overly synchronized in certain regions, almost locked up, as it tries to stabilize and reorganize itself. Instead of smooth communication, the brain produces too much crosstalk. This is especially common in the first one to two years after injury, and it often leads to difficulty multitasking, mental fatigue, and a feeling of being overwhelmed.
These combined findings, elevated slow waves, reduced fast waves, abnormal alpha patterns, and hypercoherence, painted a clear picture of a brain still struggling to recover from trauma. This explained why the patient felt foggy, slow, anxious, and visually strained, even though structural imaging showed no abnormalities.
His symptoms were real. His injury was real. And now, for the first time since the accident, he could actually see what was happening inside his own brain.
This qEEG Brain Map became the foundation for his personalized rehabilitation plan, the plan that would help him begin to improve.

How Genesis Brain Institute Delivers Personalized Rehabilitation for Brain Injuries
Once the qEEG Brain Map revealed exactly how the patient’s brain had been affected by the accident, Dr. Kalambaheti designed a brain rehabilitation plan tailored to those specific findings. She believes that every brain injury is unique, so every treatment plan must be unique as well.
A one size fits all approach misses too much. A personalized approach gives the brain its best chance to heal.
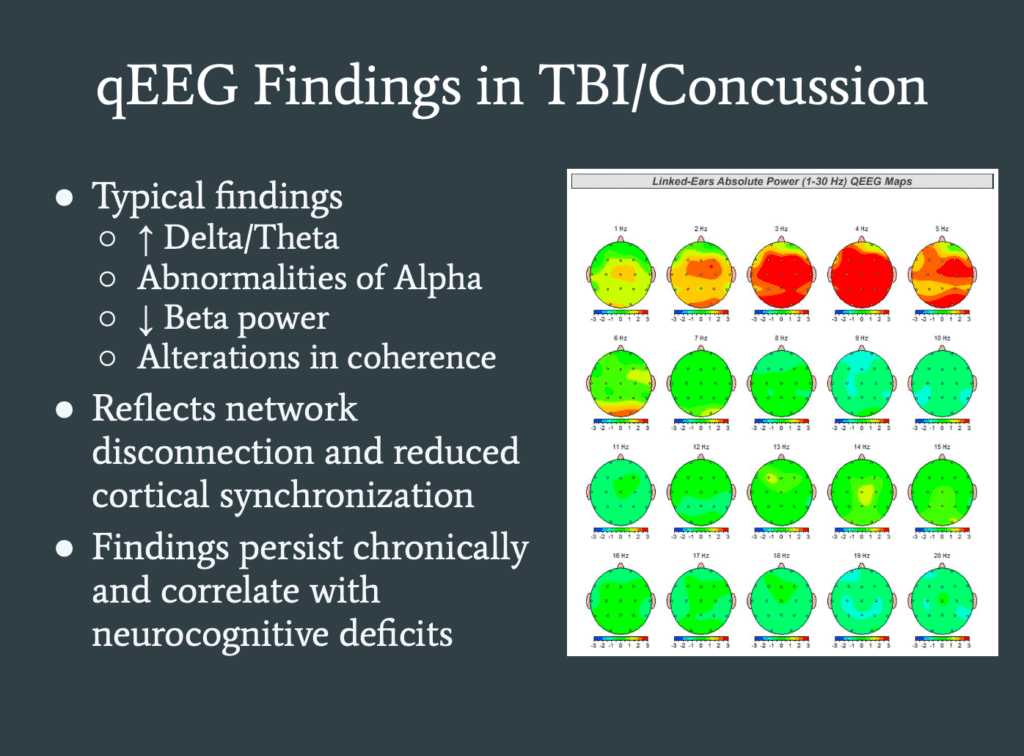
For this patient, she created a multi-modal rehabilitation program, combining several therapies that target different systems involved in thinking, balance, vision, and emotional regulation. Each therapy played a role in helping the brain recover function and stability.
The patient completed ten sessions over three months. Although Dr. Kalambaheti originally recommended ten sessions in three weeks for a more intensive schedule, he still experienced meaningful progress even with the extended timeline.
Here is the approach she used:
Hyperbaric Oxygen Therapy (HBOT)
She began each session with HBOT inside a soft chamber pressurized to 1.35 ATA with concentrated oxygen around 90% at 10 liters per minute. Each session lasted an hour, not including pressurization time. HBOT increases oxygen availability to the brain, supporting tissue healing and cellular recovery. Dr. Kalambaheti refers to HBOT as the “pre-workout” that prepares the brain for the rest of the rehabilitation session.
Transcranial Photobiomodulation (Near-Infrared Light Therapy)
Immediately after HBOT, she transitioned the patient into photobiomodulation using near infrared light at 808 to 810 nanometers. She used the qEEG map to determine which brain regions needed increased blood flow and activation. The device is applied directly to the scalp to reduce scatter and ensure the light reaches the targeted tissue.
Vagus Nerve and Median Nerve Stimulation
She incorporated electrical stimulation of the vagus nerve to help calm the nervous system and support regulation. She also stimulated the median nerve, partly because the patient had wrist dysfunction and partly because median nerve activation interacts with systems involved in consciousness and alertness. This technique has shown promise in research for individuals with severe brain injuries, and in this case, it supported improved clarity and reduced brain fog.
Vestibular Rehabilitation
Because the patient reported dizziness and balance problems, she used vestibular exercises to retrain the inner ear and balance systems. Simple viewing exercises and controlled head and eye movements helped restore stability and reduce motion related discomfort.
Virtual Reality Biofeedback
To address anxiety and autonomic dysregulation, she incorporated VR-based biofeedback. This allowed the patient to practice heart rate variability, breath control, and nervous system regulation inside an immersive environment. Calming the autonomic system is important for people recovering from TBIs because stress can intensify symptoms.
Oculomotor (Eye Movement) Rehabilitation
Using video ocularography, Dr. Kalambaheti identified how the patient’s eyes were functioning in both dark and light conditions, including pursuits, saccades, convergence, divergence, and visual reflexes. After identifying where the strain and dysfunction were occurring, she assigned specific eye exercises to strengthen the muscles around the eyes and improve visual processing. Eye movement rehabilitation is essential when a TBI affects visual clarity and stamina.
Neuromuscular Re-Education
She completed each session with neuromuscular re-education exercises designed to restore coordinated movement between the eyes, neck, and brainstem pathways. These small but important exercises support overall neurological integration and help stabilize improvements made during the session.
Dr. Kalambaheti describes this multi-modal approach as the best part of her job, watching patients begin to feel better as the brain receives targeted support in multiple areas.
Each therapy prepares the brain for the next, creating a layered effect that helps restore electrical balance, improve communication between regions, and rebuild lost function.
This personalized plan became the foundation of the patient’s progress. And after completing his sessions, the results were clear.
The Patient’s Results: Improvements in TBI Symptoms After Rehabilitation for Brain Injuries
After completing ten rehabilitation sessions at Genesis Brain Institute in Tampa, the patient experienced meaningful and measurable improvements. Dr. Kalambaheti explained that the goal of treatment is not just to help someone feel better, but to create real, observable changes in how the brain functions. In this case, both happened.
The first sign of progress came from the patient himself. He reported clearer thinking, reduced visual strain, better balance, and less cognitive fatigue. The heavy fog he had felt since the accident began to lift. Tasks that were overwhelming became manageable again. He felt more present, more stable, and more like himself.
These changes were confirmed with measurable data. At the beginning of treatment, he scored a 22 on the Rivermead Post-Concussion Questionnaire, which falls into the range associated with post-concussional syndrome. Six of his symptoms were rated as severe, meaning they affected him daily. After treatment, his total symptom score improved by roughly 40 percent, and the number of symptoms rated as severe dropped from six to just two.
Equally important were the improvements seen on his qEEG Brain Map. The elevated slow-wave activity that matched his fogginess began to normalize. His depressed beta activity, which reflected difficulty with processing and cognitive speed, strengthened. The hypercoherence across different regions began to settle as the brain regained healthier, more efficient communication patterns.
In simple terms, the electrical activity inside his brain shifted toward more normal functioning. Slow waves that were too high lowered. Fast waves that were suppressed increased. And the networks that were over connected began to organize themselves more effectively.
His improvements did not mean every symptom disappeared, but they showed that his brain was healing. Even the symptoms he still felt were different, they reflected musculoskeletal injuries, not neurological dysfunction. As Dr. Kalambaheti often tells her patients, when brain-related symptoms improve and physical pain becomes the main focus, that is still a sign of real progress.
Most importantly, he left with confidence. He could see the improvements on his brain map. He could feel the difference in his day to day life. And for the first time since the accident, he understood why he had been struggling and why he was finally getting better.
This case demonstrates what becomes possible when a brain injury is measured correctly and treated with a personalized, multi-modal brain rehabilitation plan. The next step is understanding why personalization matters so much in traumatic brain injury recovery.
Why Personalized Rehabilitation for Brain Injuries Matters
One of the strongest themes in Dr. Kalambaheti’s work is that no two brain injuries are the same. Even if two people experience the same type of accident, the effects on their brain can look completely different. The electrical activity may change in different regions, different networks may become disrupted, and symptoms can vary widely from person to person. Because of this, she stresses that a traumatic brain injury cannot be treated with a generic or standardized brain treatment plan.
Personalization matters because the brain itself is personal. Dr. Kalambaheti often explains that each person’s brain is as unique as their fingerprint. When an injury occurs, the disruption that follows is also unique. One patient may show excessive slow wave activity. Another may show depressed fast waves. Another may have severe hypercoherence or visual system overload. Without measuring these patterns, it is impossible to know what that patient truly needs.
This is why qEEG Brain Mapping is central to her approach. It provides a precise view of how the brain is functioning, which areas are struggling, and which networks need support. Instead of guessing or relying only on symptoms, she uses objective data to design a treatment plan that fits the individual.
Personalized rehabilitation also matters because people recover differently. Some respond quickly to vestibular therapy. Others improve most with photobiomodulation or nerve stimulation. Some need heavy focus on visual retraining, while others require autonomic regulation to feel safe and stable again. A dynamic, individualized strategy allows the right therapy to be used at the right time.
Dr. Kalambaheti also emphasizes that rehabilitation must be adaptive. As the brain changes during treatment, the plan should evolve with it. A therapy that is needed in the early phase may no longer be needed later. Another therapy may become more important as symptoms shift or as coherence normalizes. By continuously evaluating progress, she ensures that each session moves the patient closer to better function.
This personalized approach also gives patients something many lose after a traumatic injury: a sense of direction. Instead of being told “your scan is normal” or “your symptoms will go away eventually,” they now have a clear map of what is happening inside their brain and a targeted plan to support healing. This clarity alone can restore confidence, reduce fear, and help people feel hopeful again.
Ultimately, personalized rehabilitation works because it respects the fact that the brain heals in its own way and on its own timeline. By tailoring care to the individual, Dr. Kalambaheti creates shorter treatment plans, bigger improvements, and outcomes that truly matter to the patient. This TBI case study is a powerful example of what becomes possible when brain injuries are not just treated, but truly understood.
The Role of qEEG Brain Mapping in Guided Rehabilitation in Long-Term Recovery
One of the biggest challenges for people recovering from a traumatic brain injury is knowing whether they are actually improving. Symptoms can feel unpredictable. Some days are better, some days are worse, and many patients have no way to tell if their brain is truly healing or just coping. This is why a qEEG guided brain rehabilitation plays such an important role in long-term recovery.
Because qEEG measures the brain’s electrical activity, it shows whether the therapies being used are actually helping the brain return to healthier patterns. Instead of guessing, hoping, or relying only on symptom changes, Dr. Kalambaheti uses the qEEG brain map to confirm whether the brain is stabilizing, communicating more effectively, and producing more balanced brainwave activity.
This matters because recovery is not always obvious. Someone may feel small improvements that don’t yet translate into daily life. Others may feel stuck even though their brain is beginning to reorganize internally. qEEG allows both the clinician and the patient to see what is happening beneath the surface so treatment can stay on track.
qEEG also plays a crucial role in deciding what to do next. If slow waves are still elevated, treatment can continue targeting those regions. If beta waves begin to normalize but coherence problems remain, therapy can shift toward network stabilization. If visual processing is still impaired, more oculomotor rehabilitation may be needed. The brain is constantly adapting, and the qEEG helps rehabilitation adapt with it.
This is what makes long-term recovery more efficient. When the treatment plan is built around objective data, progress becomes faster, clearer, and more predictable. Patients do not waste time on therapies they do not need. Instead, they receive targeted interventions that match their exact patterns of injury.
Most importantly, qEEG guided brain rehabilitation gives patients confidence during a time when confidence can be hard to find. They can see the changes on their brain map. They understand why certain therapies are being used. They can visualize their progress instead of guessing. This turns recovery from a mystery into a measurable, guided process.
For many patients, that clarity is life-changing. When you finally understand what happened inside your brain, and you can see it improving, you regain a sense of control over your future. You no longer feel lost in your symptoms. You feel supported, informed, and hopeful.
This is why qEEG is more than a diagnostic tool. It is a roadmap for recovery, a way to track healing, and a guide that helps the brain rebuild function step by step. It shows the injury, it guides the treatment, and it confirms the progress that follows.
What This TBI Case Study Means for Anyone Still Struggling After a Car Accident
For many people, the hardest part of recovering from a car accident isn’t the pain, it’s the confusion. They know something feels wrong, yet every test comes back normal. They try to push through headaches, fogginess, anxiety, visual strain, or balance problems, but nothing seems to change. Over time, they begin to wonder if they’re imagining their symptoms or if they’re simply “stuck this way.”
This TBI case study shows something different. It shows that hidden brain injuries are real. It shows that symptoms have a cause. And it shows that recovery becomes possible when the brain is measured correctly and treated in a personalized way.
The patient in this case had a normal MRI, yet he had real neurological changes affecting his daily life. He struggled with cognitive fog, balance issues, visual strain, and anxiety, and his symptoms affected him every day. The qEEG Brain Map revealed patterns that explained exactly what he was feeling. It showed elevated slow waves, reduced fast waves, and hypercoherence patterns commonly seen in traumatic brain injuries. Once these patterns were identified, a multi-modal brain rehabilitation plan helped him improve by about 40 percent.
This matters for anyone who is still suffering after an accident because it proves that symptoms have a source and that the brain can heal. It shows that when someone says, “I just don’t feel like myself,” there is often a measurable reason behind it. And more importantly, there is a path forward.
This case also highlights something hopeful: improvement does not take years. With the right plan, targeted therapies, and personalized care, meaningful changes can happen in weeks or months, not decades. Even if symptoms have lingered, even if previous tests were normal, and even if someone feels frustrated or overlooked, this case demonstrates that recovery is possible.
It also shows the power of data. Seeing the brain’s electrical activity gives patients the clarity they’ve been missing. It takes away the uncertainty that so often follows a TBI. Instead of guessing, they can see what changed, why it changed, and how treatment is helping.
For anyone still struggling after a car accident, this TBI case study offers a clear message: you are not broken, you are not imagining your symptoms, and you are not out of options. Your brain may simply need a personalized rehabilitation approach, one built on measurement, technology, and a deep understanding of how the brain heals.
There is hope. And with the right tools, the right team, and the right plan, you can begin to feel like yourself again.
The Final Takeaway: Hope, Healing, and the Future of Rehabilitation for Brain Injuries
Rehabilitation for brain injuries has entered a new era. For decades, people with lingering symptoms after car accidents had little clarity and even fewer answers. They were told to “wait it out,” try medication, or accept that their symptoms were just part of life now. But this TBI case study and the science behind it, show something very different.
When the brain is measured with qEEG brain mapping, hidden injuries can finally be seen. When those findings guide a personalized rehabilitation plan, the brain can begin to reorganize, rebalance, and heal. And when treatment focuses on the individual instead of a one size fits all program, recovery becomes faster, clearer, and far more effective.
This is the future of traumatic brain injury care in Tampa. It is data-driven. It is science-backed. It is personalized. And most importantly, it gives people their lives back no only in Tampa, but those who fly in from around the country.
The Tampa patient in this case saw measurable improvements in symptoms, brainwave patterns, and daily function. He went from feeling foggy, strained, and overwhelmed to feeling clearer, steadier, and more capable. The changes on his qEEG matched the changes he felt and that alignment brings something that no medication or generic protocol can replace: confidence.
This approach matters because millions of people are living with symptoms that have never been properly understood. They are not getting worse because they are weak. They are not stuck because their injury is permanent. They are struggling because their brain injury was never measured at the level where it exists: inside the brain’s electrical networks.
Rehabilitation for brain injuries works when it starts with clear data, a personalized plan, and a team that understands how the brain heals. It works when brain treatment targets the visual system, the balance system, the autonomic system, and the electrical activity itself. It works when qEEG guides every step, ensuring that each therapy pushes the brain in the right direction.
And most importantly, it works because the brain is capable of change. Even after trauma. Even after months of symptoms. Even when other tests show nothing.
This is the message patients need to hear:
You are not stuck. Your symptoms make sense. Your brain can heal. And with the right brain rehabilitation plan, you can feel like yourself again.
At Genesis Brain Institute in Tampa Bay, this is not a theory, it is something we see every week. With the right tools and the right approach, recovery is no longer a mystery. It becomes a measurable, hopeful, and achievable path forward.
Your brain has a story. qEEG brain mapping in Tampa helps us read it. Personalized brain rehabilitation helps us change it. And your healing becomes possible again.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Please consult with a licensed healthcare provider. Genesis Brain Institute is a Brain Treatment Center in Tampa offering non-pharmaceutical solutions that bring clarity, restore function, and offer real hope for those who feel lost, stuck, or simply want more from life.